Taking Action on Childhood Cancer Prevention
For the last 50 years, the incidence of childhood cancer has been steadily rising in the United States. The amount of concern among scientists and medical professionals that environmental chemicals are contributing to the rising cancer rates has also been growing.
An important new report released yesterday by the Childhood Cancer Prevention Initiative finds “cross sector” opportunities for doctors, scientists, businesses, and policymakers to reduce hazardous chemicals entering the environment and preventing cancer:
While adults and young people can breathe in, swallow, and absorb hazardous chemicals through their skin, children face added risks through maternal or paternal transfer of toxics. Reducing production and use of chemicals that can cause cancer is an opportunity for childhood cancer prevention.
Even though survival rates of children diagnosed with cancer have improved thanks to exciting breakthroughs in research and treatments, pediatrician and public health expert Philip Landrigan, M.D., knows very well that “childhood cancer is a dreaded disease”:
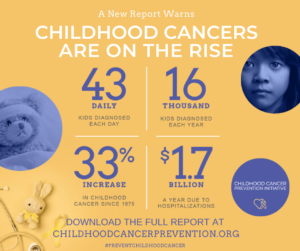
In 2019, more than 16,000 children in the United States were diagnosed with cancer. These children have leukemia, brain cancer, kidney cancer, bone cancer and more. Fifteen percent of them will not survive beyond five years. Cancer is now the largest cause of death from disease in American children.
In the foreword to Childhood Cancer: Cross-Sector Strategies for Prevention, Dr. Landrigan observes that despite falling death rates, the incidence of childhood cancer — the number of new cases per 100,000 children — has been steadily increasing in the United States:
Since the mid-1970s, cancer incidence rates in American children have increased sharply. From 1975 to 2017, leukemia incidence rates increased by roughly 34%, and incidence rates of brain and other central nervous system cancers increased 40%.
These increases are too rapid to be due to genetic change. They cannot be explained by increased access to medical care or by improvements in diagnosis. Recognition is growing that hazardous exposures in the environment are powerful causes of cancer in children.
Yesterday on The PediaBlog, we examined a list of chemical contaminants that may contribute to cancer in children and adults. Dr. Landrigan adds a few more:
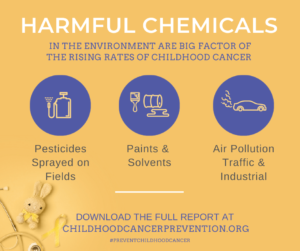
Maternal exposure to ionizing radiation such as X-rays during pregnancy, and early childhood exposures to CT-scans, have been found to increase risk of childhood leukemia and brain tumors. Prenatal exposure to diethylstilbestrol (DES) causes adenocarcinoma of the vagina in female fetuses. In more recent years, robust evidence has emerged for other links, including traffic-related air pollution, paints, and solvents such as benzene, which elevate risks of leukemia, lymphoma and brain tumors. Prenatal exposures to pesticides are associated with increased incidence of leukemia. Children living in communities surrounded by manufacturing facilities, refineries or intensive agriculture—where residents are often low-income or people of color—may have particularly high exposures.
There are three sources of chemicals that generate the highest concern regarding the development of pediatric cancer. The hopeful fact is that exposure to these risk factors can be significantly reduced:
- Air pollution, especially traffic-related pollution but also emissions from fixed, industrial sources. Some carcinogenic air pollutants, including benzene, formaldehyde, and 1,3-butadiene, are strongly linked with childhood cancer, and are emitted from vehicles and factories. The risk is heightened in children who begin breathing polluted air at a young age.
Potential avenues of action for reducing the risk of cancer from ambient air pollution include transitioning away from diesel- and gasoline-run vehicles, enforcing no-idling laws, and siting new schools and homes away from busy roadways and factories. Monitoring emissions and holding industrial polluters accountable by enforcing laws and regulations designed to protect public health would go a long way in reducing air pollution and cancer risk.
- Pesticides used on crops and at home. Occupational and residential exposure to insecticides, herbicides, and fungicides in either parent before conception, during pregnancy in the mother, and early in life has been linked to the development of leukemia, lymphoma, and brain cancer in children.
Pesticides are toxic by design and therefore more dangerous in children. They shouldn’t be used where children live, go to school and play (especially on lawns), and where pregnant mothers can be exposed. Parents should explore alternative methods of insect control in and around the house that don’t involve toxic chemicals. In Pennsylvania, schools are required to implement Integrated Pest Management, which alerts parents, teachers, and staff before chemical pesticides are applied. Additional regulations like this one are likely to reduce exposure to pesticides in children.
- Indoor chemical exposures, especially paints and solvents. Current research links parental exposures and maternal exposures during pregnancy to increased pediatric cancer risk. Benzene is an example of a commonly used solvent associated with cancer in adults and children. A component of oil and natural gas, benzene is used as a solvent in fracking operations and is a chemical byproduct when fossil fuels are burned.
Other indoor carcinogens include outdoor air pollution infiltrating indoor air, radon gas (the second-leading cause of lung cancer after tobacco smoke), toxic off-gases like formaldehyde coming from building materials, furniture, and flooring, and chemicals contained in cleaning products, disinfectants, and cosmetics.
While most other advanced countries apply the precautionary principle and test their products for safety and toxicity before they enter the marketplace, the U.S. takes the reactionary approach which doesn’t protect anyone, especially children.
More than 85,000 chemicals are in use by industry and consumers in the United States. Very few of them have actually been tested for safety or toxicity in adults, and practically none of them have been studied in children. Yet there is growing concern that more than a few of these chemicals might be driving the increase in pediatric cancers. “We are flying blind with no instruments,” worries Dr. Landrigan. Confronting rising cancer rates in children by requiring all new chemicals and all widely used existing chemicals to be tested for safety and toxicity in children is urgently needed:
We need to launch a National Cancer Prevention Plan—a second front on the War on Cancer—a powerful program of intervention against the root causes of childhood cancer that will complement and sustain the great advances we have made in cancer treatment.
There’s a case to be made that researchers, industries, businesses, consumers, and policymakers all have an opportunity as well as a responsibility to help to solve this childhood cancer crisis in America. Dr. Landrigan knows that the health and well-being of our children is at stake:
To be successful, the National Cancer Prevention Plan needs the support of people in every sector of American society, in every region of our great country and of all political beliefs and persuasions. This plan is about our children, our values as a country, and ultimately about our future.
Parents are often unaware of children’s exposure to toxic chemicals where they live, go to school, and play. Contained in this report is new knowledge that will help parents make good choices to protect their children, including reducing exposures to toxic chemicals prior to getting pregnant or during pregnancy, not just during the first years of life.
Unfortunately, many sources of toxic chemicals are beyond an individual’s control. People living in southwestern Pennsylvania still breathe chemical pollution from older coal-fired power plants and steel-making facilities, as well as more recent threats to health coming from rapidly expanding fracking and petrochemical operations throughout the region.
Businesses and governments have a responsibility — and an enormous opportunity — to accelerate the reduction in the manufacture and use of toxic chemicals. Doing so gives families the best chance at a cancer-free future.
With knowledge comes responsibility. It is time to take preventative measures NOW to reduce the number of children diagnosed with cancer.
September is Childhood Cancer Awareness Month. Read the full report on childhood cancer prevention and the reasons why action is needed now, here. Watch yesterday’s press conference announcing the report’s release here.
Dr. Ketyer participates in the SWPA Cancer and Environment Network which brings together cancer-focused organizations, academics, community groups, environmental leaders, and others to follow the relevant science, and collaborate to reduce environmental carcinogens as a critical — and often overlooked — pathway for cancer prevention. Dr. Ketyer is also a member of Women for a Healthy Environment’s Science Advisory Committee. This blog is reproduced with permission.